Seeking emergency medical care in the US after a sexual assault can incur hefty hospital bills that may deter assault reporting and compound victims’ trauma, according to a new study published in the New England Journal of Medicine.
On average, hospital emergency departments charged $3,551 for urgent medical care coded as caused by sexual violence. People who were sexually assaulted while pregnant faced even steeper bills, with an average of $4,553. Uninsured victims or those who chose to pay themselves were served bills that averaged $3,673. Even those with private insurance faced burdensome bills; the study found that insured victims paid an average of 14 percent of their bills out-of-pocket, which for the average bill would work out to nearly $500.
“Emergency department charges may discourage the reporting of rape and seeking of medical care for both short-term and long-term sequelae of sexual assault,” the authors caution. “Incurring such charges may further harm survivors—even those with full insurance coverage—by serving to disclose a potentially stigmatizing event to parents, partners, or employers. Moreover, such bills may further traumatize survivors by suggesting that they are personally responsible for their assault.”
The study was conducted by researchers from across the country, including at the University of California, Los Angeles; Harvard University; City University of New York at Hunter College; and led by a physician at Planned Parenthood in Billings, Montana.
Steep price
The team sifted through nationally representative data on 35,807,950 hospital-based visits to emergency departments from the 2019 Nationwide Emergency Department Sample database. They pulled out information on visits that had at least one diagnostic code for sexual violence.
In all, they gathered records of 112,844 emergency department visits linked to sexual assault. Among the victims, 88 percent were women. Most (53 percent) were between the ages of 18 and 44 years, but 38 percent were between 0 and 17.
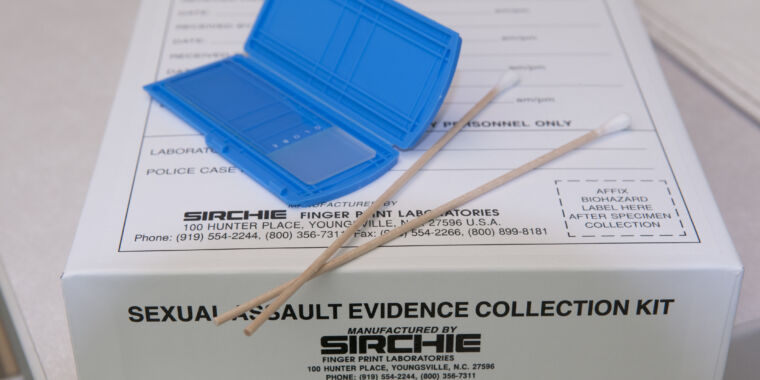
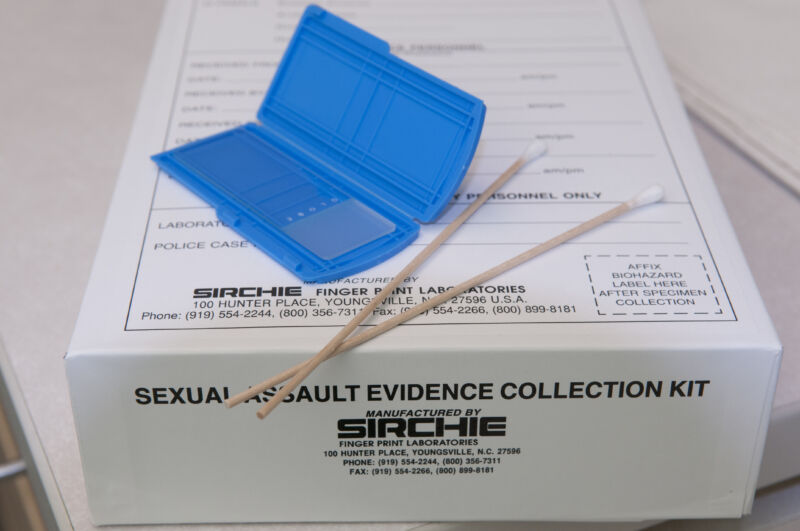
Treatments provided in these emergency care visits can include evidence collection (“rape kits”) but also treatment for physical injuries, such as broken bones or vaginal laceration repairs. There’s also diagnostic testing, treatment to prevent sexually-transmitted diseases and HIV infection, emergency contraception, and counseling.
Medicaid was the expected payer for 36 percent of the victims, and 36 percent reported income of less than $38,000. Among the 112,844 records, an estimated 17,842 victims were expected to pay their hospital bills themselves.
The authors note that the 1994 The Violence Against Women Act (VAWA) mandates that women should not be charged for evidence collection during their post-assault medical care, though that is not always heeded. But, they push further, saying that the VAWA should also cover treatment. “More extensive reforms, including universal health care coverage, are needed to ensure that costs are not a barrier to essential medical care and forensic evaluation in cases of sexual assault,” the authors argue.