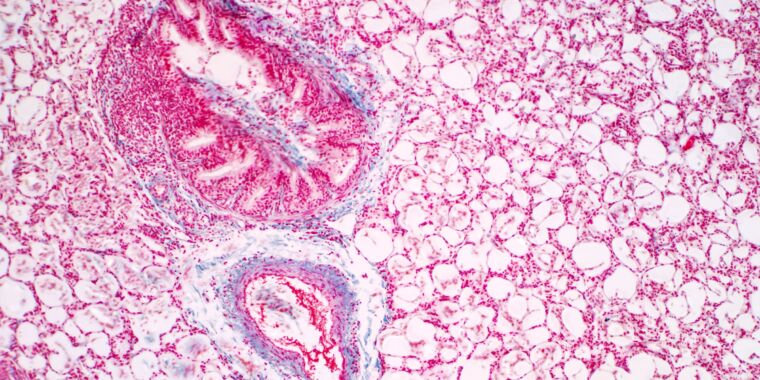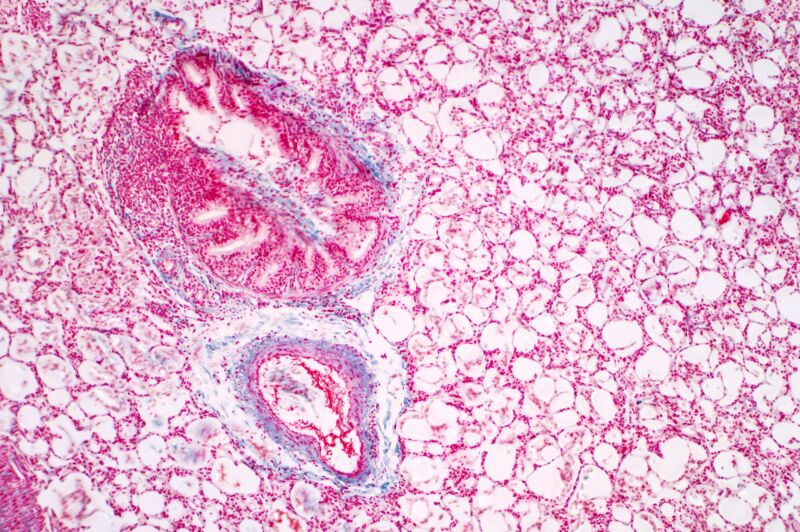
Getty Images
In a plastic-domed case at the Toronto General Hospital Research Institute, researchers gave a pair of lungs a new identity. When the lungs first arrived in the lab, they were from someone with type A blood, meaning that there were certain tiny markers, called antigens, attached to the lung tissue and blood cells. But when the lungs left the lab, those antigens were almost entirely gone. In just one hour, the researchers had effectively transformed the lungs into type O.
“This is absolutely amazing,” says Aizhou Zhang, a researcher in the Cypel Lab at the University of Toronto and first author on a paper published this week in Science Translational Medicine that describes the transformation. The experiment is an important step toward giving more people access to life-saving organ transplants. More than 100,000 people in the United States are currently waiting for organs, but often those most in need can’t get help because of one big problem: their blood type doesn’t match the organs that are available.
Zhang works in a lab run by Marcelo Cypel, lead author on the paper and a thoracic surgeon who’s spent years figuring out ways to increase the number of lungs available for transplants. One of his previous innovations was creating ex vivo lung perfusion (EVLP), that plastic-domed apparatus in which this study’s lungs got their new identity.
The device allows doctors to feed donated lungs nutrients and oxygen in a protected environment, which improves their transplant viability. Unlike organs that are put on ice after being harvested from a donor and then go straight to the operating room, lungs inside the EVLP warm up, and their metabolism restarts before they’re transplanted. Doctors can then reassess the lungs’ function and use EVLP to administer drugs that improve the quality of the organ, saving slightly damaged lungs that might have been ineligible for use before. “We put the lung back to life on this machine,” says Cypel, who thought this technology could also be used to modify the organ, transforming it into one that can be received by a person of any blood type.
There are four major blood type groups: A, B, O, and AB. Think of type O as the base model. It has no antigens that attach to it. The A and B blood types each have extra antigens that attach to that core, and AB blood has both types of antigens.
For an organ transplant to work, the donor and recipient have to have compatible blood types. If someone with type O or B blood receives a donation from someone with type A blood, for example, those A antigens will trigger the recipient’s immune system to attack the transplanted organ, which is perceived as a foreign invader. This process, called rejection, can be deadly.
But because type O blood has no antigens, people with O are considered “universal donors.” Their blood and tissue won’t set off an immune response for recipients of any blood type.
Increasing the number of universal donors, Cypel hoped, would make more lungs available to more people and make the process more equitable. “Today we have a separate list of A patients, B patients, O patients, and we don’t necessarily transplant [to] the sickest one,” he says. And even if a pair of donor lungs match the person’s blood type, they might be the wrong size for them. Too small and they won’t provide enough oxygen. Too big and they won’t fit correctly into the chest.